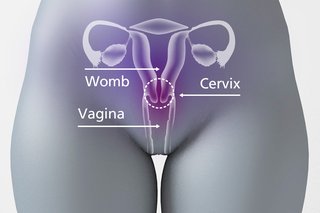
Human papillomavirus (HPV) is a common virus that 8 in 10 people will get. It usually goes away without causing any problems. Most of us will never know we had it. However, for a small number of women and people with a cervix, their immune system will not be able to get rid of HPV. Over time, this may develop into cervical cancer if not monitored or treated. Cervical screening (a smear test) checks the health of your cervix. The cervix is the opening to your womb from your vagina. It’s not a test for cancer, it’s a test to help prevent cancer.
Human papillomavirus (HPV) is a common virus that 8 in 10 people will get. It usually goes away without causing any problems. Most of us will never know we had it. However, for a small number of women and people with a cervix, their immune system will not be able to get rid of HPV. Over time, this may develop into cervical cancer if not monitored or treated. Cervical screening (a smear test) checks the health of your cervix. The cervix is the opening to your womb from your vagina. It’s not a test for cancer, it’s a test to help prevent cancer.

All women and people with a cervix between 25-49 years old should have a test every 3 years and between 50-64 years, every 5 years. Over 65 years old sh
ould only have one test if your last three tests were abnormal. If you have a cervix and have had any kind of sexual contact, with a man or a woman, you could get cervical cancer. This is because nearly all cervical cancers are caused by infection with high risk types of HPV.
You should receive a letter when you are due your cervical screening (smear test) by the NHS. When you receive this letter Book online / call our reception on 01273 772020 / fill out a Klinik Access to request an appointment.

How cervical screening helps prevent cancer
Cervical screening checks a sample of cells from your cervix for certain types of human papillomavirus (HPV).
These types of HPV can cause abnormal changes to the cells in your cervix and are called “high risk” types of HPV.
If these types of HPV are found during screening (an HPV positive result), the sample of cells is then checked for abnormal changes. If abnormal cells are not treated, they may turn into cervical cancer.
What is HPV?
HPV is the name for a very common group of viruses.
Most people will get some type of HPV during their lives. It is very common and nothing to feel ashamed or embarrassed about.
You can get HPV from any kind of skin-to-skin contact of the genital area, not just from penetrative sex.
This includes:
- vaginal, oral or anal sex
- any skin-to-skin contact of the genital area
- sharing sex toys
Some types of HPV (called “high risk” types) can cause cervical cancer. In most cases your body will get rid of HPV without it causing any problems. But sometimes HPV can stay in your body for a long time.
If high risk types of HPV stay in your body, they can cause changes to the cells in your cervix. These changes may become cervical cancer if not treated.
If you do not have a high risk type of HPV it is very unlikely you will get cervical cancer, even if you have had abnormal cell changes in your cervix before.
What happens at the appointment
During cervical screening a small sample of cells is taken from your cervix for testing.
The test itself should take less than 5 minutes. The whole appointment should take about 10 minutes.
It’s usually done by a female nurse or doctor.
Before starting, they should explain what will happen during the test and answer any questions you have.
See what the cervix is
See what a speculum and brush may look like

How cervical screening is done
- You’ll need to undress, behind a screen, from the waist down. You’ll be given a sheet to put over you.
- The nurse will ask you to lie back on a bed, usually with your legs bent, feet together and knees apart. Sometimes you may need to change position during the test.
- They’ll gently put a smooth, tube-shaped tool (a speculum) into your vagina. A small amount of lubricant may be used.
- The nurse will open the speculum so they can see your cervix.
- Using a soft brush, they’ll take a small sample of cells from your cervix.
- The nurse will close and remove the speculum and leave you to get dressed.
What your results mean
Your results letter will explain what was tested for and what your results mean.
Sometimes you’ll be asked to come back in 3 months to have the test again. This does not mean there’s anything wrong, it’s because the results were unclear. This is sometimes called an inadequate result.
Human papillomavirus (HPV) is not found in your sample
Most people will not have HPV (an HPV negative result).
This means your risk of getting cervical cancer is very low. You do not need any further tests to check for abnormal cervical cells, even if you have had these in the past.
You’ll be invited for screening again in 3 or 5 years.
HPV is found in your sample
Your results letter will explain what will happen next if HPV is found in your sample (an HPV positive result).
You may need:
- another cervical screening test in 1 year
- a different test to look at your cervix (a colposcopy)
There are 2 different kinds of HPV positive result:
| Result | What it means |
|---|---|
| HPV found (HPV positive) but no abnormal cells | You’ll be invited for screening in 1 year and again in 2 years if you still have HPV. If you still have HPV after 3 years, you may need to have a colposcopy. |
| HPV found (HPV positive) and abnormal cells | You’ll be asked to have a colposcopy. |
Information:
HPV is a common virus and most people will get it at some point. You can get it through any kind of sexual contact.
Support for everyone
For more information and support about going for cervical screening, results and treatment, you can contact Jo’s Cervical Cancer Trust by:
- joining the Jo’s Cervical Cancer Trust forum
- calling the Jo’s Cervical Cancer Trust helpline on 0808 802 8000
- using the Jo’s Cervical Cancer Trust ask the expert service
Support for people with a learning disability
Support for LGBT people
Support for people with vulval pain
Support after sexual violence
If you have experienced sexual violence, you may find the idea of cervical screening very difficult.
The My Body Back Project gives support after sexual violence by running My Body Back screening clinics for people who have experienced sexual violence.
There is also advice and support about cervical screening after sexual violence from Jo’s Cervical Cancer Trust.
Find out more about what HPV is